Abstract
Mantle cell lymphoma (MCL) is a rare chronically relapsing subtype of aggressive B-cell non-Hodgkin lymphoma characterized by the canonical chromosomal translocation t (11;14) and other molecular cytogenetic aberrations including overexpression of BCL2 protein. Venetoclax (VEN), a BCL2 inhibitor, has demonstrated activity in MCL both as a monotherapy and in combination with other targeted agents. Treatment with single agent venetoclax is, however, hampered by frequent development of drug resistance caused in large part by adaptive upregulation of other anti-apoptotic BCL2 family members.
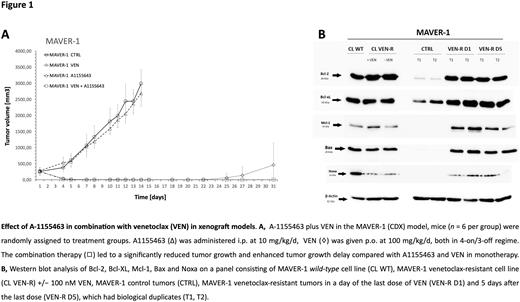
Immunodeficient NOD-SCID-gamma mice were xenografted subcutaneously with MCL cell lines and PDX cells established from patients with relapsed and refractory MCL. The therapy was given for two weeks. VEN was administered by oral gavage (100 mg/kg/d), A1155463 was administered intraperitoneally (10 mg/kg/d). Western blotting was implemented to evaluate expression levels of BCL2 proteins, immunoprecipitation was used to analyze the levels of BIM bound to BCL2 and BCL-XL before and after exposure to VEN. CRISPR-Cas9 was employed to derive clones with BCL-XL knock-out. Blood cell counts in mice on A1155463 +/- VEN therapy were analyzed using the Mindray BC-5300 Auto Hematology Analyzer.
In this study, we analyzed molecular mechanisms of in vivo acquired resistance to VEN using a panel of several murine cell line-based xenografts (CDX) and patient-derived xenografts (PDX) of MCL. First, the mice xenotransplanted with VEN-sensitive MCL cells were subject to monotherapy with VEN until development of resistant tumors (VEN-R). Western blot analysis of VEN-R tumors revealed upregulation of BCL-XL in majority of VEN-R tumors compared to controls. Other changes included upregulation of MCL1 and downregulation of BIM proteins in several models. Immunoprecipitation experiments confirmed that BCL-XL indeed serves as a buffer for BIM released from BCL2 after exposure to VEN thereby blocking VEN-triggered apoptosis. Importantly, we demonstrated that the upregulation of BCL-XL caused not only VEN resistance, but also led to BCL-XL-specific pro-apoptotic priming of VEN-R lymphoma cells. In vitro, the combination of VEN and A1155463, a specific BCL-XL inhibitor, induced cytotoxic synergy on a panel of MCL cell lines and primary cells. CRISPR-Cas9-mediated BCL-XL knock-out resulted in marked sensitization to VEN-induced apoptosis in MCL cell lines. In vivo, pharmacological blockage of BCL-XL strongly increased sensitivity to VEN. Despite that A1155463 exerted limited anti-lymphoma activity as monotherapy on tested CDX and PDX models, its combination with VEN was synthetically lethal and exerted significantly enhanced anti-lymphoma activity. The efficacy of the VEN and A1155463 combination was highly effective even in mice bearing VEN-R tumors (tumors with acquired VEN resistance, Figure 1). It has been published that mechanisms responsible for BCL-XL upregulation include activation of NFkappaB signaling via CD40 and hypoxia. Upregulation of BCL-XL induced by these factors in turn caused VEN resistance in vivo. Indeed, we confirmed that upregulation of BCL-XL was observed already after engraftment of VEN-sensitive MCL cells in immunodeficient mice. MCL cells isolated ex vivo from the established CDX tumors were significantly more sensitive to BCL-XL inhibition compared to the corresponding in vitro growing cell lines. Our results thus confirmed increased BCL-XL dependence of MCL cells in vivo compared to in vitro. We suggest that these microenvironmental factors were also critical for the selection of VEN-resistant clones during the therapy with VEN. Historically, experimental therapy of patients with chronic lymphocytic leukemia with navitoclax, a combined inhibitor of BCL2 and BCL-XL, was rater disappointing. The plausible reasons included both low efficacy of navitoclax due to insufficient BCL2 inhibition, and a dose-limiting thrombocytopenia. We demonstrated that the thrombocytopenia associated with continued therapy with A1155463 could be managed by 4 days on / 3 days off treatment strategy, which cannot be applied in case of fixed dual BCL2/BCL-XL inhibitors like navitoclax, or AZD4320.
In summary, the combined inhibition of BCL2 and BCL-XL with VEN and A1155463 is a highly effective experimental treatment strategy for R/R MCL with a potential translation to the clinical grounds.
Disclosures
Trněný:Takeda: Consultancy, Honoraria, Research Funding; Bristol-Myers Squibb: Consultancy, Honoraria; Incyte: Consultancy, Honoraria; Abbvie: Consultancy, Honoraria; Amgen: Consultancy, Honoraria; Roche: Consultancy, Honoraria, Research Funding; Gilead Sciences: Consultancy, Honoraria; Janssen: Consultancy, Honoraria; MorphoSys: Consultancy, Honoraria; Novartis: Consultancy, Honoraria, Research Funding; Zentiva: Consultancy, Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal